Discover some 2023 highlights of migraine research from the “home of neurology”
The 9th Congress of the European Academy of Neurology (EAN) took place in Budapest, Hungary, from 1–4 July 2023. This second hybrid EAN meeting was a hive of activity, offering an extensive range of cutting-edge research and the opportunity to network with colleagues from around the world. During the four-day meeting, delegates were immersed in a range of unique educational opportunities to explore ‘Neurology beyond the Big Data’ and learn about novel methods to improve the lives of those affected by headache in Europe. Read on to discover some key highlights from EAN 2023.
Key industry symposia
Targeting CGRP: Debating key clinical decisions in migraine prevention (Teva sponsored symposium)1
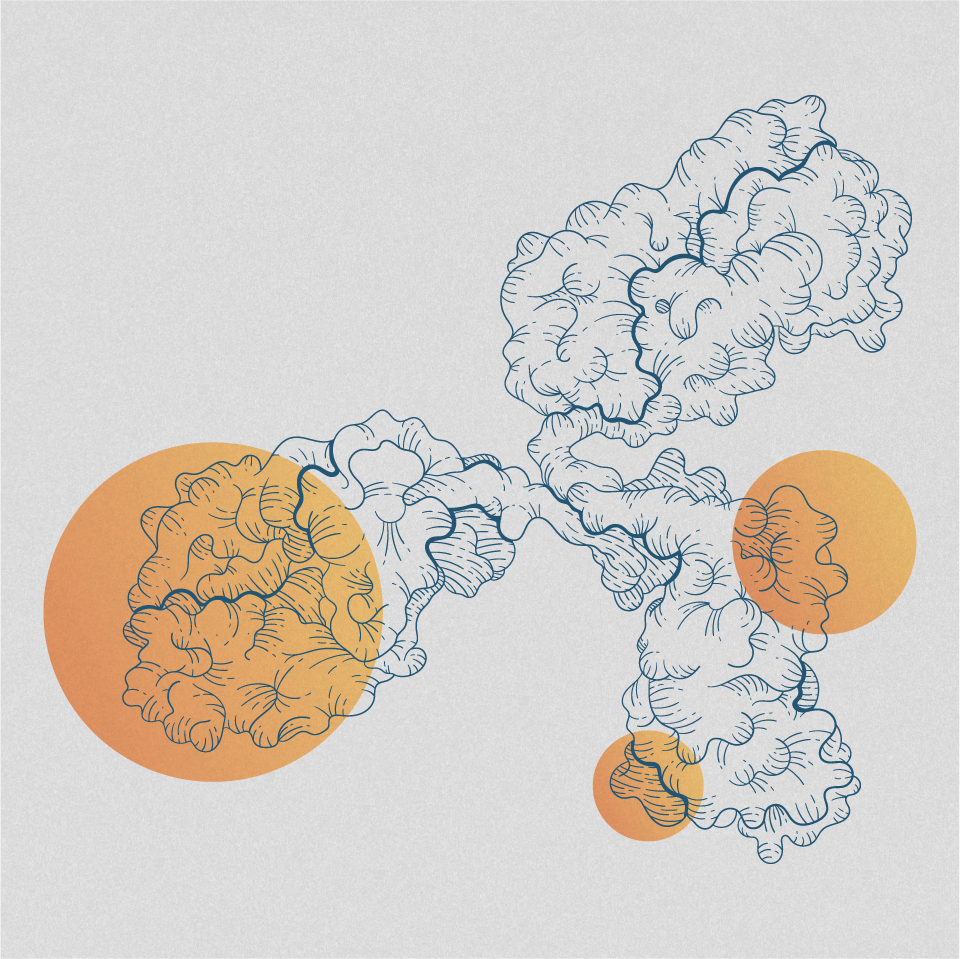
Professor Messoud Ashina introduced the programme by presenting the latest data on calcitonin gene-related peptide (CGRP) pathway monoclonal antibodies (mAbs).
Dr Claudia Altamura opened the first debate, ‘Is it better to target the CGRP ligand or receptor in migraine prevention?’ by arguing that there is no substantial difference between targeting the CGRP receptor or ligand. She noted that targeting the CGRP receptor may be beneficial for patients who do not respond to ligand-targeting treatments.
During the second debate, ‘Can psychiatric comorbidities and migraine be addressed with a single treatment?’, Dr Giorgio Lambru noted depression as a risk factor for migraine, and migraine as a risk factor for depression, arguing that the two cannot be addressed with a single treatment. He emphasised that non-migraine-specific medications may be unsuitable for patients with psychiatric comorbidities and may even exacerbate depressive symptoms; therefore, separate treatments are needed for both conditions. Dr Altamura then argued that preventive treatment for migraine may help reduce the burden of migraine and allow symptoms of depression to improve, presenting data from the Phase 3 UNITE trial, a study which aims to evaluate the efficacy and safety of a CGRP pathway mAb in adult patients with migraine and comorbid major depressive disorder.
Migraine matters: Patient perspectives and expert insights (Lundbeck-sponsored symposium)1
Professor Dawn Buse opened this session with a video of a patient describing the negative impact chronic migraine has on her quality of life (QoL).
Professor Christoph Schankin presented data highlighting the burden and progression of migraine. He emphasised that both lifestyle changes and preventive treatments were available to improve the QoL of patients with migraine; however, these are often underutilised and introduced too late in the treatment process.
Professor Jan Versijpt shared key results from several Phase 3 trials, demonstrating that CGRP pathway mAbs are effective at reducing monthly migraine days, can reduce acute medication use in comparison to placebo, without the need for detoxification and broadly improve patient-reported outcomes.
Advancing the treatment of migraine with gepants: Focus on acute treatment (Pfizer-sponsored symposium)1
Professor Simona Sacco emphasised the need for effective migraine treatments, as ineffective treatment can increase the likelihood of transition from episodic to chronic migraine compared with maximum efficacy treatment, as scored by the Migraine Treatment Optimization Questionnaire. Additionally, polypharmacy among migraine sufferers may suggest limitations in the current available therapies.
Professor Patricia Pozo-Rosich highlighted the key takeaways from the 2021/2022 EAN/European Headache Federation (EHF) consensus statement on the acute treatment of migraine and the 2022 EHF consensus, which defined the effective acute treatment of a migraine attack and triptan failure.
Professors Alan Rapoport and Simona Sacco followed by presenting further data from several Phase 3 studies of gepants to demonstrate the effectiveness of prescribing these agents for migraine prevention.
Migraine, your patient, and you: Overcoming migraine together (Eli-Lilly-sponsored symposium)1
Professor Cristina Tassorelli opened this symposium by sharing a video of a patient’s experience living with migraine, highlighting the negative impact migraine had on her QoL, and the long journey that she took to obtain a correct diagnosis and effective treatment.
Professor Zaza Katsarava discussed the burden and stigma related to migraine.
Professor Manjit Matharu summarised results from several online discrete choice experiment surveys examining the largest drivers of patient preference in episodic or chronic migraine, noting that markers of efficacy were the most important to patients. He highlighted the importance of considering patient experience in clinical decision-making, particularly with the expanding preventive treatment options available.
Optimizing individualised migraine care (AbbVie-sponsored symposium)1
Professor Cristina Tassorelli opened by highlighting the low levels of evidence for the use of non-targeted oral preventive treatments in patients with chronic migraine. She presented data on the low adherence to and failure of oral migraine preventive treatments. She concluded her presentation by noting that the EHF guidelines include CGRP pathway mAbs as a first-line treatment option.
Professor Patricia Pozo-Rosich subsequently presented data from Phase 3 trials evaluating the efficacy and safety of atogepant in patients with episodic and chronic migraine. She also presented the estimated economic savings associated with a ≥50% reduction in monthly migraine days, and the economic savings associated with this. She argued that the early initiation of preventive therapies is the next biggest challenge in migraine management and machine learning could help overcome this barrier.
This session included several polling questions for the audience to voice their opinions on migraine preventive treatments. Insights were obtained on the availability and utility of migraine management guidance, access to and utility of targeted therapies, preferences for treatment formulation (oral versus injection), and evidence for the use of CGRP pathway mAbs and neuromuscular blockers in migraine.
Key scientific sessions
Neurology by night: The role of sleep pathology in neurological disorders1
Dr Rolf Fronczek presented an overview of headache disorders defined by attacks in the night. He briefly explained the symptoms of exploding headache syndrome and hypnic headache. The glymphatic system, a macroscopic waste system, functions during sleep and is largely inactive during wakefulness. During a migraine attack, there is inflammation in the glymphatic system involving CGRP; therefore, Dr Fronczek hypothesised that if a patient was to sleep, the pro-inflammatory mediators could be removed. Lastly, Dr Fronczek presented data on cluster headache, which appear to be seasonal for patients with episodic cluster headache. He discussed the link between cluster headaches, sleep and hormone levels, including lower levels of melatonin during attacks. There is a potential link between the frequency or worsening of cluster headache and a higher number of daylight hours.
CGRP antagonists should be the drugs of choice for migraine1
Professor Messoud Ashina opened by presenting evidence to support the use of CGRP pathway mAbs as a first-line treatment for migraine. He discussed the challenges of non specific oral migraine preventives, including delayed efficacy, poor tolerability and high discontinuation rates, and stated that targeted preventives can overcome such barriers.
Professor Ashina highlighted efficacy data for CGRP pathway mAbs from Phase 3 trials, showing significant improvements versus placebo across a range of endpoints, including high responder rates, rapid onset and sustained long-term efficacy. He noted that these improvements were also observed across patient subgroups who typically do not respond well to treatment.
Professor Cristina Tassorelli argued that CGRP pathway mAbs should only be used after trialling several other drugs, as cost rules them out as first-line treatment. She noted that adverse events experienced with traditional oral preventives are not life-threatening or persistent events, yet lower adherence impacts the overall effectiveness. She proposed that treatment of migraine is linked to relevant comorbidities.
A new era of migraine treatment: What is right for our patients?1
Professor Simona Sacco first compared CGRP pathway mAbs to conventional oral migraine preventives, highlighting the benefits of CGRP pathway mAbs in reducing medication overuse and noting that the early adoption of CGRP-targeting preventives may be beneficial in preventing not only this, but disease progression and refractoriness. She highlighted that it is important to remember there will be non-responders to CGRP pathway mAbs, and recommended combination with other pharmacological agents or non-pharmacological interventions (such as neuromodulation, physical activity or cognitive behavioural therapy).
Next, Dr Giorgio Lambru explored neuromodulation as an alternative or add-on treatment option to pharmacological treatments in primary headaches, including single pulse transcranial magnetic stimulations, External Trigeminal Nerve Stimulation and remote electrical neuromodulation. These treatments can be particularly beneficial for patients who do not tolerate, respond or have contraindications to established and novel acute therapies, however, there are a lack of real-word data for these treatments, which is the main barrier to developing these further.
Dr Irene de Boer closed the symposium by using case studies to explain how to diagnose and treat hemiplegic migraine, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy, retinal vasculopathy with cerebral leukoencephalopathy and systemic manifestations and Dutch-type cerebral amyloid angiopathy.
Multicenter real-world case-control study of effectiveness, tolerability and anti-CGRP response predictors in the elderly1
Dr Alicia González Martínez set the scene for her oral presentation by stating that elderly patients are more likely to have comorbidities and polypharmacy and could therefore benefit from therapies with better tolerability profiles. To date, there are limited data regarding efficacy and safety of CGRP pathway mAbs in patients 65–75 years old. She presented data on CGRP pathway mAb effectiveness in elderly patients (>65 years), with no significant differences in tolerability observed between the elderly patient group and the control group (<55 years of age).
1. 9th Congress of the European Academy of Neurology; July 1–4, 2023; Budapest, Hungary.